GLP-1 Therapy Part 3: Strategies for Successful Weight Loss
I recently had the pleasure of speaking at the Colorado Academy of Nutrition and Dietetics Annual Conference on the topic of nutrition strategies for effective GLP-1 use in obesity treatment.
This premier event, dedicated to supporting nutrition and dietetics professionals in Colorado, offered a valuable opportunity to share updated evidence on GLP-1 therapies, while also debunking common myths to promote informed and unbiased nutrition counseling.
In this four-part series, I’m excited to share my key recommendations to help support your practice. In Part 3, we’ll discuss strategies for successful weight loss while on GLP-1 therapy, as well as the transition into maintenance.
New to this series? Start with Part 1: Setting Realistic Weight Loss Expectations and Part 2: Preventing and Managing Side Effects.
Nutrition as the Foundation for Success
While GLP-1 therapy provides significant metabolic benefits, including weight loss, its long-term effectiveness depends largely on complementary changes in nutrition and eating behaviors.
When combined with therapeutic nutrition and the adoption of a balanced, sustainable eating pattern, individuals can improve overall health and maintain weight loss—sometimes even while reducing or eliminating the need for ongoing medication (more on that in Part 4).
Targeted nutrition strategies help reinforce progress, supporting both the rate of weight loss and long-term success.
Protein
Adequate protein is vital for promoting satiety through hunger-inhibiting hormones like leptin, increasing thermogenesis, and supporting skeletal muscle retention—ultimately helping to maintain or increase basal metabolic rate (BMR).
A daily intake of 1.2–1.5 grams per kilogram of body weight is recommended (excluding those with renal conditions). Use actual body weight for individuals with a BMI under 30, ideal body weight for BMI 30–40, and adjusted body weight for BMI over 40.
Aim for at least 50% of protein from whole food sources, supplementing as needed. Choose protein supplements based on individual needs: whey protein isolate for weight or muscle support, casein for glucose management, hydrolyzed whey for those with GI issues or gastroparesis, and pea protein for plant-based preferences.
Fiber
The recommended daily fiber intake is about 14 grams per 1,000 calories consumed, translating to at least 25 grams per day for women and 38 grams per day for men. Reaching these targets can support good digestive health, help prevent medication-related side effects, and enhance satiety.
Fluids
Aim to consume 2–3 liters (over 10 cups or 80 ounces) of fluid per day. Ideal choices include water, coffee or tea, herbal infusions, low-fat milk (dairy or plant-based), and beverages that are low in calories, added sugars, and caffeine—keeping total caffeine intake under 400 mg per day.
Developing Healthy Eating Patterns
Above all, this is the time to establish a healthy, sustainable eating pattern. Focus on a protein- and produce-forward approach that includes lean proteins (animal or plant-based), non-starchy fruits and vegetables, whole grains, lower-fat dairy options, and heart-healthy fats.
Avoid restrictive diets and instead prioritize food quality over quantity. A multivitamin may be considered if needed.
Calorie guidelines from the American Heart Association, American College of Cardiology, and The Obesity Society suggest 1,200–1,500 kcal/day for women and 1,500–1,800 kcal/day for men, though individual needs may vary. Practice tuning into hunger and fullness cues and lean into intuitive eating.
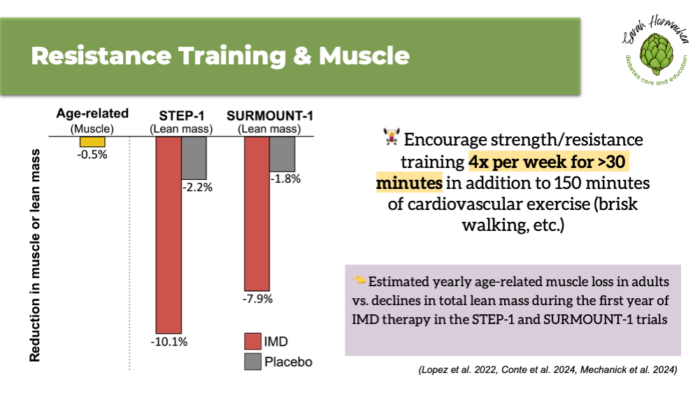
Protecting Muscle During Weight Loss
Changes in lean skeletal muscle mass are an important consideration during rapid weight loss. Resistance training, along with adequate protein intake, is a vital strategy for preserving lean muscle—particularly in the context of aging and hormonal changes.
Encourage patients to engage in structured resistance training at least four times per week for a minimum of 30 minutes per session, in addition to 150 minutes of cardiovascular exercise, such as brisk walking.
Key Takeaways
Successful weight loss with GLP-1 therapy is most effective when paired with evidence-based nutrition strategies that promote sustainability, preserve lean muscle mass, and support metabolic health.
Emphasize adequate protein, fiber, and fluid intake, alongside a balanced eating pattern, to enhance satiety and minimize side effects. Encouraging resistance training and mindful eating behaviors further reinforces long-term success.
By integrating these core strategies into your practice, you can better support patients in achieving meaningful and lasting outcomes with GLP-1 therapy.
Stay tuned for Part 4 next week, where we’ll dive into key considerations for medication discontinuation and maintaining long-term metabolic health and weight loss.
- Moon J, Koh G. Clinical Evidence and Mechanisms of High-Protein Diet-Induced Weight Loss. J Obes Metab Syndr. 2020;29(3):166-173. doi:10.7570/jomes20028
- Spreckley M, Seidell J, Halberstadt J. Perspectives into the experience of successful, substantial long-term weight-loss maintenance: a systematic review. Int J Qual Stud Health Well-being. 2021;16(1):1862481. doi:10.1080/17482631.2020.1862481
- U.S. Department of Agriculture and U.S. Department of Health and Human Services. Dietary Guidelines for Americans, 2020-2025. 9th Edition. December 2020. Available at DietaryGuidelines.gov.
- Almandoz JP, Wadden TA, Tewksbury C, et al. Nutritional considerations with antiobesity medications. Obesity. 2024;32(9):1613-1631. doi:10.1002/oby.24067
- Jensen MD, Ryan DH, Apovian CM, et al. 2013 AHA/ACC/TOS guideline for the management of overweight and obesity in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and The Obesity Society. Circulation. 2014; 129(25 Suppl 2): S102-S138.
- Lopez P, Taaffe DR, Galvão DA, et al. Resistance training effectiveness on body composition and body weight outcomes in individuals with overweight and obesity across the lifespan: A systematic review and meta-analysis. Obes Rev. 2022;23(5):e13428. doi:10.1111/obr.13428
- Conte C, Hall KD, Klein S. Is Weight Loss-Induced Muscle Mass Loss Clinically Relevant? JAMA. 2024 Jul 2;332(1):9-10. doi: 10.1001/jama.2024.6586. PMID: 38829659.
- Mechanick JI, Butsch WS, Christensen SM, et al. Strategies for minimizing muscle loss during use of incretin‐mimetic drugs for treatment of obesity. Obesity Reviews. Published online September 19, 2024:e13841. doi:10.1111/obr.13841

You May Also Like

Your Guide to Diabetes Supplies: Insulin Pens
July 4, 2023
Your Guide to Diabetes Supplies: Glucometers
June 4, 2023