GLP-1 Therapy Part 2: Preventing and Managing Side Effects
I recently had the pleasure of presenting at the Colorado Academy of Nutrition and Dietetics Annual Conference on the topic of nutrition strategies for effective GLP-1 use in obesity treatment.
This premier event, dedicated to supporting nutrition and dietetics professionals in Colorado, offered a valuable opportunity to share updated evidence on GLP-1 therapies, while also debunking common myths to promote informed and unbiased nutrition counseling.
In this four-part series, I’m excited to share my key recommendations to help support your practice. In Part 2, we’ll discuss strategies for managing and preventing medication-related side effects
New to this series? Start with Part 1: Setting Realistic Weight Loss Expectations
Nutrition Therapy for Side Effects
GLP-1 therapy can be an immensely impactful class of medication for obesity treatment and improving metabolic health—but it only works if you can tolerate it. Adverse side effects are one of the leading reasons individuals discontinue therapy or are unable to increase their dose, even if they haven’t yet reached their desired goals.
Thankfully, strategic nutrition therapy can play a key role in preventing and reducing these side effects. The most commonly reported side effects of GLP-1 therapy include nausea, vomiting, constipation, diarrhea, bloating, burping, and dizziness.
Smaller, More Frequent Meals
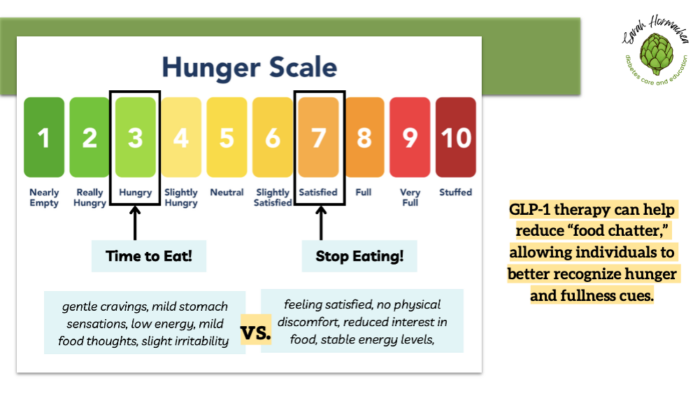
Encourage patients to eat 5–6 smaller meals throughout the day to help minimize nausea and reduce the risk of vomiting. Advise them to avoid overeating and to stop eating when they feel comfortably full. Introducing the concept of a hunger/fullness scale can support mindful eating and help patients better recognize satiety cues. This approach may also help reduce symptoms such as belching or sulfuric (sulfur-like) burps.
Increased Fluids
Increasing fluid intake is essential for managing constipation, diarrhea, nausea, and vomiting. Encourage patients to aim for at least 10 cups (80 oz or 2.5 liters) of fluids per day.
To help prevent dehydration, consider incorporating oral rehydration solutions (ORS) such as coconut water, broth, or diluted juice with a pinch of salt. Advise patients to limit fluid intake 30–60 minutes before and after meals to help reduce feelings of fullness and nausea.
Fiber for Regularity
Adequate fiber intake is important for supporting regular bowel movements and reducing constipation. Encourage patients to aim for 25–35 grams of fiber per day through a combination of whole foods such as fruits, vegetables, whole grains, legumes, and nuts.
For individuals who struggle to meet their fiber needs through diet alone, supplementation with psyllium husk or methylcellulose can be helpful. Increasing fiber gradually can improve tolerance and effectiveness.
Reducing Dietary Fat
Limiting dietary fat can help reduce nausea, reflux, and prolonged feelings of fullness. High-fat meals are known to slow gastric emptying, which can worsen symptoms such as nausea and acid reflux.
Patients may benefit from counseling on low-fat food swaps and cooking methods, such as grilling, baking, or steaming instead of frying. Those following high-fat dietary patterns, like keto, may require additional guidance to adjust their intake while maintaining nutritional balance.
Complementary Therapies
Don’t underestimate the effectiveness of homeopathic and complementary treatments in managing side effects like nausea and vomiting.
- Herbal teas and chews containing ginger, peppermint, chamomile, or lemon can provide gentle relief and are generally well-tolerated.
- Aromatherapy using essential oils such as lavender, spearmint, cardamom, or clove may also help ease discomfort and promote a sense of calm.
- Acupressure—commonly used in oncology and pregnancy care—can be a non-invasive option to help reduce nausea and improve overall comfort. These strategies can be supportive tools alongside nutrition and medication adjustments.
When Nutrition Therapy Isn’t Enough
If nutritional strategies aren’t sufficient to manage side effects, consider recommending over-the-counter medications. Products like Pepto-Bismol or Kaopectate may help with general gastric discomfort, while Dramamine can be useful for nausea or dizziness.
For more persistent symptoms, a short-term prescription of Zofran (ondansetron) may provide relief as the body adjusts to GLP-1 therapy. If side effects persist, consider down-titrating to a lower dose for a longer period to allow for better tolerance and gradual adaptation.
Key Takeaways
Side effects are common with GLP-1 therapy but often manageable with proactive support. Nutrition therapy is a first-line tool for improving tolerance—small, frequent meals, adequate hydration, increased fiber, and reduced dietary fat can all make a difference.
Complementary strategies like herbal teas, aromatherapy, and acupressure can provide additional relief. When symptoms persist, over-the-counter or prescription medications may be helpful as the body adjusts.
As always, remember to tailor recommendations to the individual’s lifestyle, preferences, and tolerance.
Stay tuned for Part 3 next week, where we’ll explore specific nutrition-based strategies to support weight loss while on GLP-1 therapy.
- Gorgojo-Martínez JJ, Mezquita-Raya P, Carretero-Gómez J, et al. Clinical Recommendations to Manage Gastrointestinal Adverse Events in Patients Treated with Glp-1 Receptor Agonists: A Multidisciplinary Expert Consensus. J Clin Med. 2022;12(1):145. Published 2022 Dec 24. doi:10.3390/jcm12010145
- Academy of Nutrition and Dietetic: Nutrition Care Manual. Nausea And Vomiting Nutrition Therapy. https://www.nutritioncaremanual.org/client_ed.cfm?ncm_client_ed_id=23. Accessed April 24, 2024

You May Also Like

Entrepreneurship in Diabetes Care and Education
November 26, 2024
The Value of the Diabetes Educator
June 27, 2022