
4 Clinical Pearls from the 2024 ATDC Conference
I was very fortunate to attend the 2024 ATDC Conference this year in beautiful Keystone, Colorado. The ATDC Conference has been an integral part of education and case-based studies of pipeline diabetes technology for over 30 years. This year’s focus included keynotes and plenaries on topics such as cardiovascular disease outcomes in both type 1 and type 2 diabetes, early detection strategies, updates in AID and Rx/OTC sensors, updates in macro- and microvascular complications, and even a possible cure for type 1 diabetes.
Despite being an intimate event, hosted at almost 10,000 feet, there was no shortage of big names in diabetes research. I am excited to share four of the trending topics that truly challenged my knowledge and assumptions about diabetes care and education.
#1. A1c is wrong—but that doesn't mean it isn't useful
We’ve known for a while now that Hemoglobin A1c (HbA1c) has its pitfalls. There are many people for whom it’s simply inaccurate. Used to estimate the percentage of hemoglobin (the protein in red blood cells) that is glycated (coated with sugar), it is based on the assumption that RBCs live for about 90 days before turning over. However, we’re realizing that there is much greater heterogeneity in real life.
Pregnancy, anemia, thalassemia, sickle cell disease, chronic kidney or liver disease, dialysis, alcohol use, age, and other hemoglobinopathies can all affect A1c accuracy. Even healthy adults can have a falsely elevated A1c given that the lifespan of RBCs ranges from 70 to 140 days, with an average of 115 days. So why are we using an inherently inaccurate tool to make a life-changing diagnosis?
It turns out, we might just be using it to answer the wrong question. Rather than serving as a marker of glycemic control, it may actually tell us about our risk of microvascular complications.
“Fast glycators” are individuals for whom sugar attaches itself much more quickly to red blood cells. A recent study showed a correlation between glycation rates (or ratio) and diabetes-related complications, such as retinopathy and nephropathy. To calculate the glycation ratio, divide the GMI (glucose management indicator from a CGM) by the A1c. The lower the GR, the higher the glycation rate, and the greater the association with complications.
#2. A dual or "double" diabetes diagnosis is not a typo
Seeing a patient with both a type 1 and type 2 diabetes diagnosis in their medical record used to drive me up the wall. What’s up with these doctors? Don’t they know how to make a diagnosis? Are they confusing the patient? Just pick one—you can’t have both… or can you?
As it turns out, many clinicians are using a dual diagnosis as a means to get coverage for prescriptions only approved for type 2 diabetes. There are next to no adjunctive therapies approved for type 1 diabetes. But that doesn’t mean patients with type 1 diabetes are any less susceptible to overweight or obesity, cardiovascular and renal disease, postprandial excursions, and even insulin resistance.
A type 1 diagnosis as the etiology and a type 2 diagnosis for prescriptions often opens the door to effective and life-changing treatment.
#3. Hypercortisolism as a cause of uncontrolled diabetes
Preliminary results from the recently published CATALYST study showed that 1 in 4 individuals with difficult-to-control type 2 diabetes actually have hypercortisolism, a condition characterized by high cortisol levels. Among these patients, many were found to have a cortisol-producing adrenal adenoma, a noncancerous growth that is not often screened for during routine diabetes care.
Excess cortisol levels were associated with increased insulin resistance and worsening glycemic control and hyperglycemia. Without treatment for hypercortisolism (either surgical or pharmacological), patients were at a much greater risk for adverse cardiovascular outcomes.
I wouldn’t be surprised if the next iteration of the standards of care includes screening and monitoring for cortisol levels in patient with worsening glycemic control.
#4. Less the 26% of people with T1D are at target (A1c <7.0%)
This number astounded me. Despite all the new automated and adaptive technologies, early screening tools, advancements in care, and growing awareness of the disease, more than three-quarters of people living with type 1 diabetes are experiencing disruptive, uncomfortable, and even life-threatening glucose values.
It highlights the bottleneck nature of access and accessibility. What good are all these phenomenal tools if people can’t get them, or worse, can’t keep receiving them?
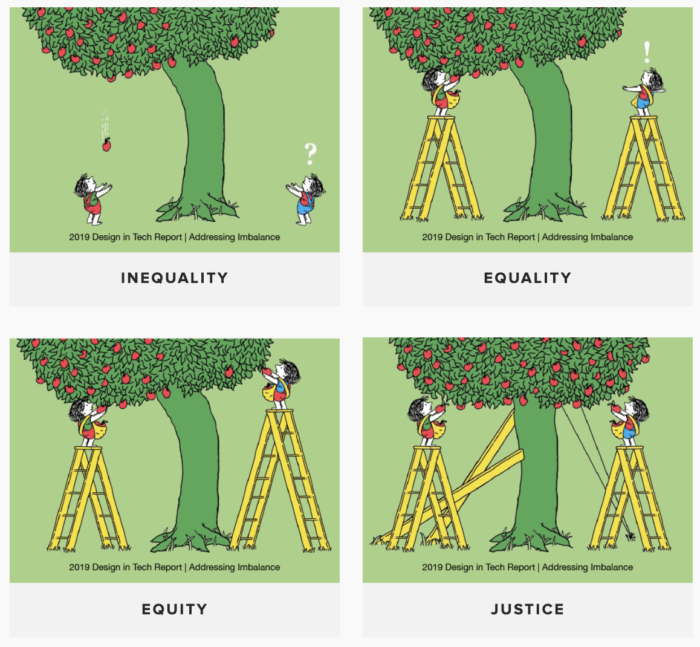
Dr. Ananta Addala, a pediatric endocrinologist at Stanford, shared her interpretation of health equity and access through the lens of The Giving Tree. It’s similar to the image we often see of kids looking over a fence to watch a baseball game (I’m sure you know the one!), except the final picture depicts how “justice” could help fix the system to offer equal access to both tools and opportunities. It has me thinking about my role as both a clinician and an advocate for diabetes care and education specialists.
Key Takeaways
The 2024 ATDC Conference in Keystone highlighted significant advancements and challenges in diabetes care. I was blown away by the quality of speakers, the breadth and depth of discussions, and the cutting-edge nature of the topics. A few key takeaways:
- Recognize the limitations of A1c as a marker of glycemic control, but consider its potential as a marker of risk for microvascular complications.
- Consider dual diabetes diagnoses as a strategy to access more comprehensive treatment options.
- Screen for hypercortisolism in those hard-to-manage diabetes cases.
- Reflect on your role in advocating for better access to diabetes care and education tools.
I am looking forward to attending ATDC again in 2025!


You May Also Like

Embracing JOMO: Finding Peace in Professional Life
December 10, 2024
Fatty Liver on the Rise: What You Need to Know
February 18, 2025
