Move Over A1c, Make Room for Time In Range
A hemoglobin A1c test (HbA1C) has long been the gold standard for diagnosis and treatment of diabetes. It’s cheap, quick, and easy to interpret. An A1c of 6.5% or greater is considered diagnostic criteria for diabetes, while 7.0% or less is regarded as controlled once diagnosed. Completed every 3-6 months, A1c is an accessible and affordable way to monitor long term glycemic control.
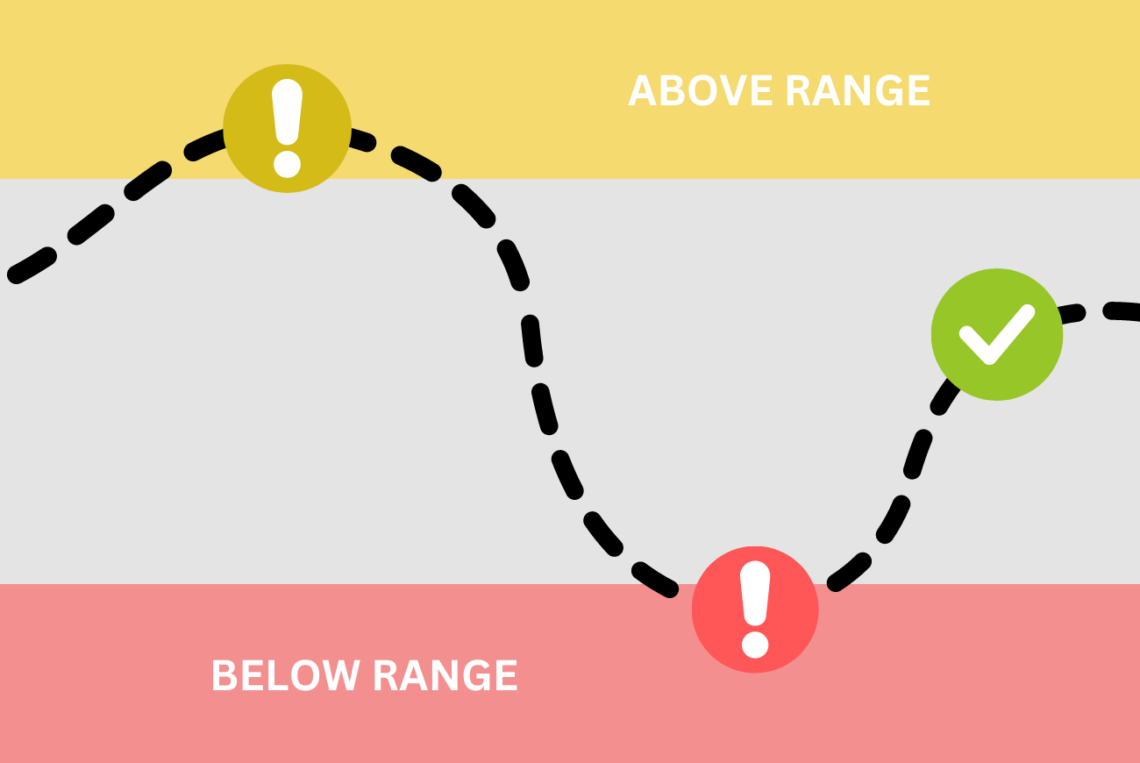
Yet, A1c often fails to capture the nuance of day-to-day management for so many people living with diabetes. A sleepless night of lows (less than 70 mg/dL) followed by a frantic day of highs (greater than 180 mg/dL) can still yield an average glucose of 140 mg/dL. This translates to an estimated A1c of 6.5%, which seems good, right? Yet, anyone living with diabetes will tell you that riding a blood sugar rollercoaster is simply exhausting. So, why are we still using A1c to evaluate glycemic control?
Time in Range
The American Diabetes Association suggests using a newer metric called Time in Range (TIR) to evaluate optimal glucose control. TIR is the amount of time an individual spends in the target glucose range—between 70 and 180 mg/dL for most people. TIR can be collected using personal CGM, professional CGM, or through a series of strategically collected fingerstick glucose data points.
Dr Tamara Oser MD and Dr Sean Oser MD, of the CU School of Medicine Primary Care Diabetes Lab, provide wonderful recommendations on how to use and interpret time in range data.
Time in Range can be used independent of hemoglobinopathies, individuals undergoing blood transfusions, or for those whom A1c seems to be consistently inaccurate when compared to fingerstick data.
Individualizing Time in Range
The exact range – and time in that range – may vary depending on the unique needs of the population.
For Type 1 Diabetes/Type 2 Diabetes:
- Greater than 70% of the time should be spent between 70-180 mg/dL
- < 4% below 70 mg/dL, with <1% below 54 mg/dL
- < 25% above 180 mg/dL, with <5% above 250 mg/dL
For the Older or Higher Risk T1D/T2D Population:
- Greater than 50% of the time should be spent between 70-180 mg/dL
- <1% below 70 mg/dL, with 0% below 54 mg/dL
- <10% above 250 mg/dL
Pregnancy
- Greater than 70% of the time should be spent between 63-140 mg/dL
- <4% of the time below 63 mg/dL, with <1% below 54 mg/dL
- <25% of the time above 140 mg/dL
Should we give up on A1c as a valid glycemic metric?
Probably not. As aforementioned, it’s cheap, quick, and easy. It doesn’t require access to personal or professional CGM. It is widely recognized and understood. However, if providers have the opportunity to order or review TIR, their overall assessment of a patient’s glycemic control is likely to be much more accurate.
Additional References:
Grunberger G, Sherr J, Allende M, et al. American association of clinical endocrinology clinical practice guideline: the use of advanced technology in the management of persons with diabetes mellitus. Endocrine Practice. 2021;27(6):505-537. doi:10.1016/j.eprac.2021.04.008
Battelino T, Danne T, Bergenstal RM, et al. Clinical targets for continuous glucose monitoring data interpretation: recommendations from the international consensus on time in range. Diabetes Care. 2019;42(8):1593-1603. doi:10.2337/dci19-0028


You May Also Like

ADCES24: Let the Good Times Role!
August 14, 2024
CDCES and Primary Care: A Healthy Partnership
June 21, 2022
